Our well-rounded revenue cycle management income summary services prioritize denial management and timely AR follow-up to streamline reimbursements for your practice. Therefore, file accurate claims and receive effective ICD-10 and CPT coding assistance. Additionally, comprehensive documentation by our EMR experts helps practices keep track of patient documentation with impeccable confidentiality standards.
Focus on Denial Management
Payment status indicator (SI) is a code used in accounts receivable in healthcare healthcare revenue cycle management to indicate the current payment status of a claim or transaction. Packaging is the process of grouping healthcare services or procedures together under a single code for billing and reimbursement purposes. Modifier is a two-digit code used in medical billing to provide additional information or clarification about a service or procedure performed by a healthcare provider.
Smart Healthcare IT Budgeting: From $1M to $10M+
The route from delivering treatment to receiving payment consists of multiple phases. Understanding and implementing these steps correctly ensures smooth revenue flow and minimizes delays in payment collection. Also known as the complete record of a patient that is sent to a healthcare provider and/or insurance agency. Educate patients about payment policies, their financial responsibilities, and the importance of timely payments. Implement a structured follow-up process for unpaid claims and patient balances.

Employer-based health insurance
Not only physicians and medical practices have changed to different working styles, processes, and technologies, insurance companies have transformed as well. Insurance companies are devising new plans to compete in a saturated market with insurance plans that can paint a desirable picture for buyers. They are offering insurance coverage with low premiums but higher deductibles. In doing so, they are adding up new requirements and regulations to make it difficult for claimants to get their payments. To ensure this, insurance companies are using sophisticated technologies that can easily detect a fault in the claims.

Hire A Medical Billing Company
Most commonly, it can be due to unauthorized service, wrong medical codes, mismatched patient information, missing documents, or a problem with physician credentialing. In the last stage, make corrections and provide all that is required by the insurance company and resubmit the claim. The medical billing professionals of Sybrid MD are proficient in handling all types of claims, insurance companies, and medical specialties.
- Payments received from payers or patients are posted to the appropriate accounts.
- Disease management is a systematic approach that focuses on preventing and controlling chronic illnesses through coordinated healthcare interventions.
- Providers charge for every service they provide; a model that at times causes over testing for reimbursement.
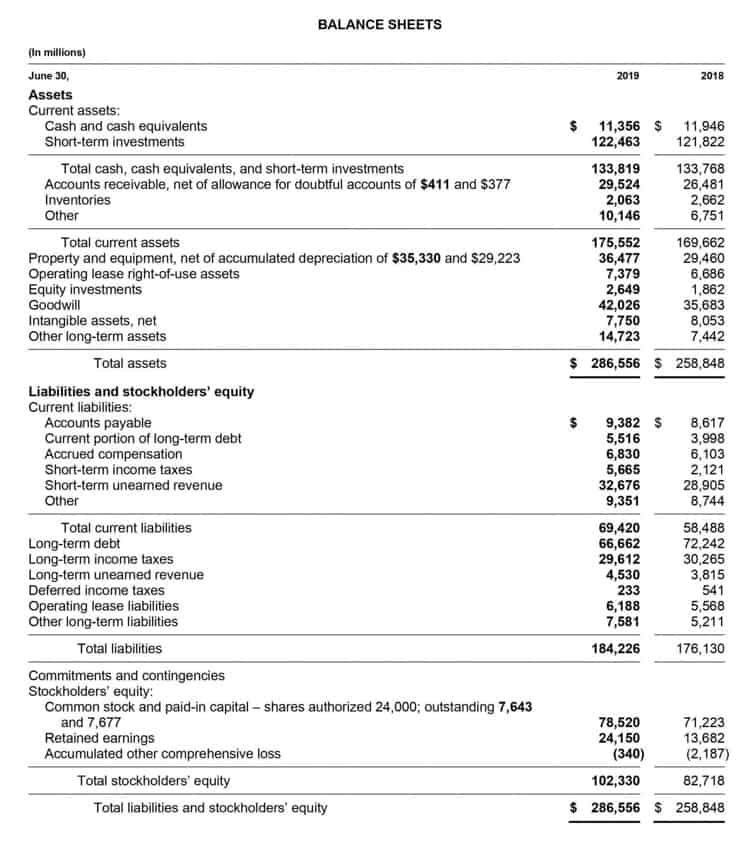
- Calculating AR days is important for understanding your medical practice’s cash flow and financial position.
- When you outsource your AR, you gain access to specialized billing professionals who focus exclusively on collections and follow-up.
- In this evolving landscape, knowing exactly what AR in medical billing stands for will remain key to financial survival and success.
- Offering patient financing options and interest-free payment plans can help you collect more money upfront.
- Unlike accounts payable, which are amounts a provider owes to others, AR represents money flowing into the organization.
- Learn how healthcare practices manage and recover money owed for patient care, crucial for their financial stability and operations.
- You’ll need to be fast on your feet in terms of understanding services, procedures, and complex insurance terms.
In conclusion, the AR, which stands for Augmented Reality in technology, Accounts Receivable in finance, and Army Rifle/Assault Rifle in defense, is a crucial term for students and professionals. Understanding each meaning of AR ensures success in exams, interviews, and career growth across industries. Proper insurance verification and obtaining pre-authorizations avoid payment delays and reduce administrative burdens later. You may forget the more obscure codes of services that aren’t done very often, but you’ll need to remember as much as possible for a smoother day and faster processing speed. Members get the flexibility to see in- or out-of-network doctors like a PPO, but their share of the costs will be higher.
- Identify and address any payment issues quickly to avoid delays in your cash flow.
- Monitoring AR performance is essential to comprehending a healthcare organization’s financial situation.
- Resource-based relative value scale (RBRVS) is a payment methodology used to determine reimbursement rates for medical services based on the resources required to provide them.
- The remaining $200 becomes part of the accounts receivable balance until it is collected from the insurance company.
- It encompasses all the payments from patients, insurance companies, and other third-party payers due to the healthcare provider.
With latest software implementation, you can minimize the risk of errors and increase the accuracy of your billing process. Additionally, medical billing software provides https://puertoricocarfreight.com/future-value-growth-compound-amount-factor/ real-time insights into your AR performance, allowing you to identify and address issues quickly with AR automation. AR is crucial for ensuring timely revenue collection, maintaining cash flow, identifying issues with claims or payments, and optimizing the financial health of a healthcare practice.
